Persistent pain is complicated and we don’t fully understand why some people develop persistent long term pain and others do not.
Persistent pain is often due to a combination of factors, these include:
- A chronic condition, such as osteoarthritis
- An initial injury - most injuries heal after three months.
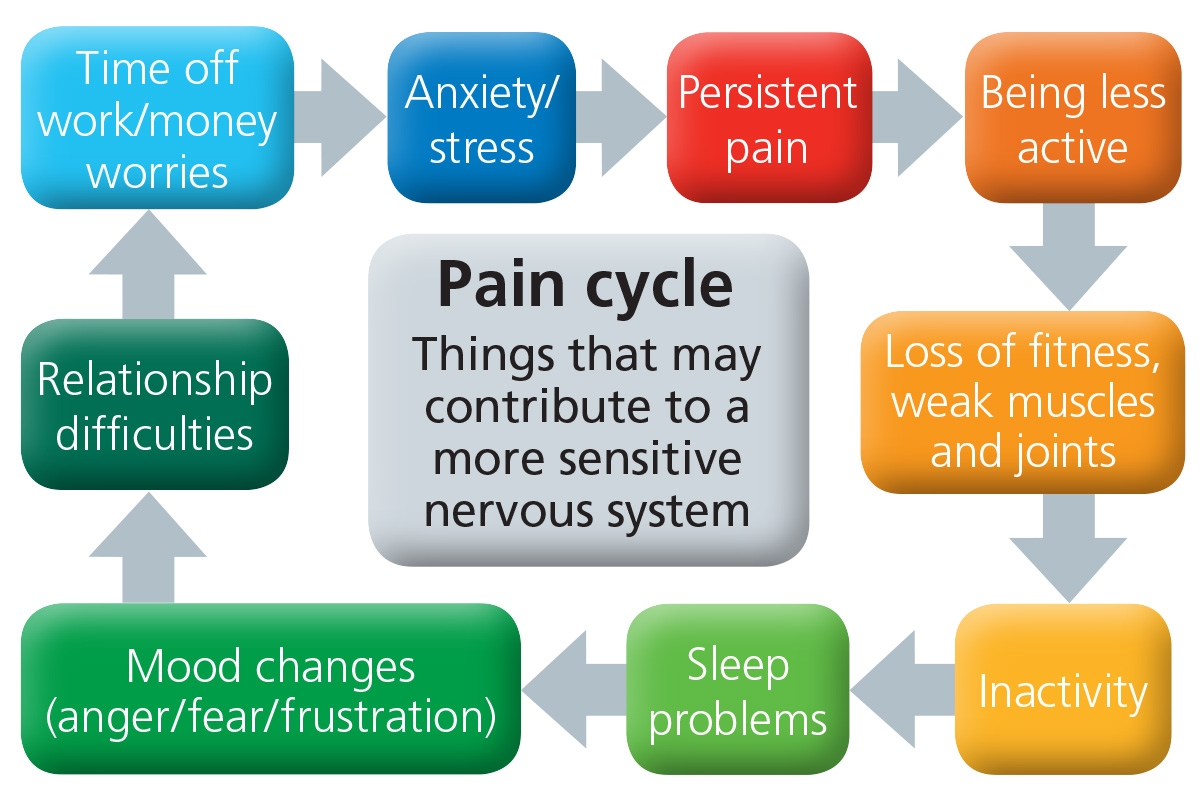
- Increased sensitivity of the nervous system. The nervous system becomes so sensitive that it reacts quicker and needs fewer stimuli to generate a painful response. Pain often extends beyond the initial injury or site of pain because joining nerves also become stimulated and don’t turn off. Normal movement can become painful
- Pain often causes a change in activity level and how we move - this often leads to stiffer and more painful joints and muscles, which can contribute to pain.
- Pain can causes low mood, anxiety, anger, stress, weight gain, lack of sleep, all of these factors then increase pain, increase the sensitivity of the nervous system and affect our ability to cope with the pain.
Persistent pain management involves looking at all of the factors that contribute to your pain.