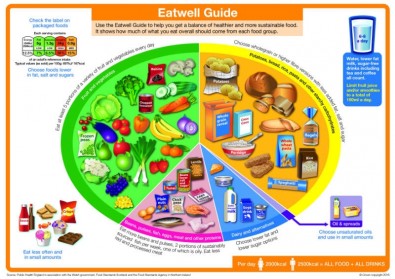
The Eatwell Guide
The Eatwell Guide can help you get a balance of healthier foods. It can be used by people with health conditions. In the past diet advice has been different e.g. for diabetes, kidney conditions, arthritis, mental health and mood.
Advice given by a specialist may be different to the Eat Well Guide. In these cases, people should follow their specialist’s advice.
To eat a healthy balanced diet, eat a variety of different foods from each section of the Eat Well Plate and, in the right portions.
Potatoes, bread, rice, pasta and other starchy carbohydrates
Starchy foods are an important part of each meal. Try to have 5-6 portions per day if you are female, 6-8 per day if you are male. Try to choose the wholegrain types as these will help you feel fuller for longer. These foods contain B vitamins which help release energy from the food we eat and help the body to work properly.
Controlling your intake of carbohydrates can help to reduce your blood glucose levels and help to keep them steady. To achieve this, eat similar portions of carbohydrates from meal to meal.
Example:
Breakfast: wholegrain cereal (2 portions)
Lunch: jacket potato (2 portions)
Evening meal: cooked rice 4-5 tablespoons (2 portions)
|
Starchy Carbohydrate |
Measure |
Portion |
|---|---|---|
|
Corn Flakes |
4-5 Tablespoons |
2 |
|
Bran Flakes |
4-5 Tablespoons |
2 |
|
Chapati |
Small |
1 |
|
Chapati |
Large |
2 |
|
Pitta Bread |
1/2 |
1 |
|
Wheat Biscuits |
2 Biscuits |
2 |
|
Porridge |
4-5 Tablespoons |
2 |
|
Chips |
4-5 Chips |
1 |
|
Chips |
8-10 Chips |
2 |
|
Potatoes |
Egg Size |
2 |
|
Jacket Potato |
Fist size |
2 |
|
Bread |
Medium slice |
1 |
|
Bread Roll |
One |
1 |
|
Cooked Rice |
4-5 Tablespoons |
2 |
|
Crisp Breads |
Two pieces |
1 |
|
Cream Crackers |
Three |
1 |
|
Cooked Pasta |
4-5 Tablespoons |
2 |
|
Cooked Spaghetti |
4-5 Tablespoons |
2 |
Fruits and Vegatables
1 portion of fruit or vegetable is approximately one handful.
Try to have at least 5 different types per day. During weight loss ensure you have the correct portion size of fruit and spread them out during the day. These foods are full of essential vitamins and minerals which help protect us from life threatening diseases such as heart disease, diabetes, cancer, kidney disease, liver disease. Fruit and vegetables can be tinned (ideally in natural juice rather than syrup), frozen or fresh.
Example:
Breakfast: chopped banana on cereal
Lunch: mixed salad in or with a sandwich
Evening meal: 2-3 different types of vegetables
Snacks: Mid-morning (1 portion of fruit)
Mid-afternoon (1 portion of fruit)
|
Fruit and Vegetable |
Measure |
Portion |
|---|---|---|
|
Carrots |
½ Plate |
1 |
|
Mixed Salad |
½ Plate |
1 |
|
Fresh Orange |
150 ml |
1 |
|
Satsuma |
2 small |
1 |
|
Orange |
Handful |
1 |
|
Peas |
½ plate |
1 |
|
Ochre |
½ plate |
1 |
|
Banana |
Small |
1 |
|
Plum |
2 |
1 |
|
Apple |
Handful |
1 |
|
Mini Sweetcorn |
½ plate |
1 |
|
Broccoli |
½ plate |
1 |
|
Cherries |
Handful |
1 |
|
Raisins |
½ Handful |
1 |
|
Grapes |
Handful |
1 |
|
Cauliflower |
½ plate |
1 |
|
Sprouts |
½ plate |
1 |
|
Apricots |
2 |
1 |
|
Dried apricots |
3 |
1 |
|
Strawberries |
Handful |
1 |
Dairy and alternatives
Dairy foods are a good source of calcium, which help keep our bones strong. Try to include 2-3 portions per day. Try to choose low fat and low sugar types. Example: 3-4 cups of tea or coffee with skimmed or semi skimmed milk (1 portion)
|
Dairy and Alternatives |
Measure |
Portion |
|---|---|---|
|
Milk |
½ Pint |
1 |
|
Soya Milk |
150ml |
1 |
|
Cheese Slice |
One slice |
1 |
|
Grated Cheese |
20g |
1 |
|
Cottage Cheese |
Small Pot |
1 |
|
Low Fat Soft Cheese |
One triangle |
1 |
|
Yoghurt |
Small Pot |
1 |
|
Yoghurt Drink |
Small Pot |
1 |
Oils and spreads
Some fats are essential as part of a healthy balanced diet as they provide us with energy and some important vitamins (vitamin A and D). However, eating too much fat can be unhealthy. Saturated fats (less healthy) e.g. butter and lard are solid at room temperature and are associated with increased risk of heart disease. Unsaturated fats are liquid at room temperature and considered to be healthier fats.
Choosing mono-unsaturated spreads and oils e.g. olive and rapeseed oil helps to lower the ‘bad’ cholesterol and increase the ‘good’ cholesterol. There are also poly-unsaturated fats e.g. sunflower, soy and sesame oils.
It’s important to remember that all fats are high in energy (kcals) and portion sizes should be small.
Aim for 2-3 portions per day.
Example:
1 tsp oil per person when cooking (1 portion)
1 tsp unsaturated spread per person on bread (1 portion)
|
Oils and Spreads |
Measure |
Portion |
|---|---|---|
|
Low Fat Spread |
1 teaspoon/ 5g |
1 |
|
Mono or poly-unsaturated oil e.g. sunflower, soy, sesame |
1 teaspoon/ 5g |
1 |
Beans, pulses, fish, eggs, meat and other proteins
Protein rich foods contain essential vitamins and minerals, these foods help our body to repair itself and provide us with a strong immune system. Too many of these foods are unnecessary and may lead to weight gain if eaten in excess, therefore only 2-3 portions per day is required.
Example:
Lunch: sliced meat or tuna or beans (1 portion)
|
Beans, Pulses fish, eggs, meat and other proteins |
Measure |
Portion |
|---|---|---|
|
Eggs |
2 |
1 |
|
Bacon |
2 small rashers |
1 |
|
Sausages |
2 thin |
1 |
|
Sardines |
Tin |
1 |
|
Fish fingers |
2 |
1 |
|
Pork/ Lamb Chop |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
|
Chicken |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
|
Steak |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
|
Meatballs |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
|
White Fish |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
|
Salmon steak |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
|
Green Lentils |
X1 palm of hand |
1 |
|
Red Lentils |
X1 palm of hand |
1 |
|
Kidney Beans |
X1 palm of hand |
1 |
|
Cannelli beans |
X1 palm of hand |
1 |
|
Butter beans |
X1 palm of hand |
1 |
|
Chickpeas |
X1 palm of hand |
1 |
|
Baked Beans |
X1 palm of hand |
1 |
|
Soya Mince |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
Eat less often and in small amounts
This section now sits outside the main 'plate' section of the Eatwell guide. These foods are higher in fat and sugar and provide little nutritional value to our diet. We can still enjoy them as part of a balanced diet but it is recommended that we eat small portions of these and reduce how often they are consumed.
Example:
1 small packet of crisps (1 portion)
1 biscuit (1 portion)
|
Beans, Pulses fish, eggs, meat and other proteins |
Measure |
Portion |
|---|---|---|
|
Sugar |
1 teaspoon/ 5g |
1 |
|
Tomato Sauce/ Salad Cream |
1 teaspoon/ 5g |
1 |
|
Peanuts |
½ handful |
1 |
|
Scone |
1/2 |
1 |
|
Plain digestive |
1 |
1 |
|
Orange sponge biscuit |
2-3oz/ 50-70g/ x1 palm of hand |
1 |
|
Fun Size chocolate bar |
Fun size / 1 |
1 |
|
Biscuit bar |
one |
1 |
|
Crisps |
25-30g bag |
1 |
Drinks
Water, lower fat milk, sugar-free drinks including tea and coffee all count.
Aim to drink 6-8 glasses per day.
Note: Limit fruit juice and / or smoothies to a total of 150ml a day.
Alcohol
The maximum recommended number of units for men and women is currently 14 units a week – ideally not all in one go and at least 2 alcohol free days. A UK unit is 10ml of pure alcohol.
Adding 2-4 units per day to your usual diet can lead to an increase in weight of around 4lbs in four weeks.
|
Alcohol |
Measure |
Unit |
Calories |
|---|---|---|---|
|
Lager/ bitter |
Pint, 3.5% |
2.8 |
182 |
|
Light Spirit |
25ml, 37.5% |
1 |
120 |
|
Dark Spirits |
25ml, 40% |
1 |
55 |
|
Red Wine |
125 ml, 12% |
1.5 |
93 |
|
White Wine |
175ml, 12% |
2.1 |
130 |
|
White Wine |
Bottle |
9 |
556 |
|
Alcopop |
Small bottle, 5% |
1.4 |
200 |
|
Cream Liqueur |
45ml |
1 |
199 |
For more information and support:
One You Leeds (Eat Better, Cook Well)
Forward Leeds
If a person is worried about the amount of alcohol they drink and would like to seek professional help, contact Forward Leeds on:
- 0113 887 2477
- info@forwardleeds.co.uk
Type 2 Diabetes - A guide to snacking
Your body produces and uses insulin to help use certain foods (nutrients) in the diet called carbohydrates to provide energy. When you have diabetes the insulin your body produces is either not enough or is not working as efficiently as it should be. This is causing your blood glucose levels to rise above the normal range.
Controlling your intake of carbohydrates can help to reduce your blood glucose levels and help to keep them steady. To achieve this you could have similar portions of carbohydrates from meal to meal. One area you may want to focus on is reducing your snacks to less than 15g of carbohydrate.
You should aim to include no more than one snack between each meal. Including more than this may increase your calorie intake excessively and lead to weight gain.
Carbohydrates
Carbohydrates all break down into glucose and will affect our blood glucose levels. Foods containing carbohydrates are:
- Starchy Foods (Potatoes, Granary Bread, Takeaway food, Pasta, Rice)
- Milk and Yoghurt
- Fruit
- Food with added sugars (Cereal, Cereal Bar, Chocolate, Cakes, Biscuits)
How many carbohydrates should I be eating?
- Starchy carbohydrates are your body’s main source of energy so we recommend you include a source of these with every meal.
- Having regular carbohydrates can help to reduce your risk of hypoglycaemia (blood glucose levels below 4mmol/l).
- Ideally you should be aiming for meals to contain a similar amount of carbohydrate day to day as this will help to keep your blood glucose levels steady.
- Initially you could aim for meals to provide between
30-50g per meal and your snacks to provide less than 15g. - Your dietitian may recommend a more specific amount if you are trying to achieve a particular goal.
What carbohydrate free snacks could I include?
- Nuts (plain or roasted) - one small handful.
- Cheese (a matchbox sized portion of hard cheese).
- Lettuce wraps - you could try filling these with meat fish or salad and a small amount of low calorie or vinaigrette dressing.
- Eggs - 2 eggs a day is a reasonable portion.
- Avocado - you could try stuffing these in a similar way to the lettuce wraps or turning them into guacamole. 1/2 an avocado is one portion.
- Vegetable sticks with 2-3 tablespoons of hummus / guacamole / salsa.
- Edamame beans with a light coating of your choice of spice / herbs.
- Any plain meat or fish for example chicken breast, ham, prawns, tinned tuna.
- Olives or gherkins.
- Omelette (made with very little milk). You could add any vegetables / meat to this.
Tip - Any of these snacks can be mixed together to make up 15g of carbohydrate. But remember that including too many snacks may lead to weight gain if your calorie intake is increased too high. Speak with your dietitian if you are unsure of how many snacks you could include for your needs.
Sweet Food (Containing 15g or less carbohydrate)
| Type of food | Amount of carbohydrates (grams) |
|---|---|
| 1 x bourbon, chocolate digestive, custard cream, ginger biscuit, oreo | 8-9 |
| 3 x party rings, malted milk, nice, rich tea |
15 |
| 1 x plain digestive | 10 |
| 1 x mini muffin | 14 |
| 1 x medium handful of any fresh fruit | 15 |
| 20g popcorn (2 x handfuls) - sweet or salted | 13 |
| 1 tablespoon peanut butter | 4 |
| Small yoghurt 100kcals or less | 15 or less |
| 74g of blueberries or strawberries (one medium handful) + 4 tablespoons crème fraiche |
11 |
| 2 x rings of tinned pineapple (juice drained) | 8 |
| Light hot chocolate made with water | 5 |
| Small ice lolly (80ml) | 15 |


 The LEEDS Programme is an education programme for people newly diagnosed with type 2 diabetes. The course covers information about Type 2 diabetes and how a carefully controlled diet, exercise and lifestyle changes can help to prevent longer term complications.
The LEEDS Programme is an education programme for people newly diagnosed with type 2 diabetes. The course covers information about Type 2 diabetes and how a carefully controlled diet, exercise and lifestyle changes can help to prevent longer term complications. 

